Experiencing trauma can cause a person to experience certain kinds of disruptions in their daily actions, distress with respect to their thoughts, feelings and emotions, and dysfunctional ways of coping. While each of us who have gone through trauma are unique in the way we have been impacted, a lot of us are at the high risk of enduring Post-Traumatic Stress Disorder symptoms, listed by the Anxiety and Depression Association of America as:
- Re-encountering the traumatic event through tedious recollections.
- Experiential avoidance and emotional numbness.
- A heightened sense of reaction, characterised by a problem in sleeping and being easily annoyed or frustrated.
PTSD, a common occurrence post-traumatic experience, has similar symptoms with another type of mental health concern – Borderline Personality Disorder (BPD). These shared symptoms include:
- Difficulty in coping with and handling uncomfortable emotions.
- Interpersonal ineffectiveness.
-
Prone to impulsive behavior.
Dialectical Behavior Therapy for PTSD
An increasingly popular treatment evidence-based treatment for BPD is Dialectical Behavioral Therapy (DBT). Given the symptoms they share, researchers have discovered the model of DBT, an effective approach to treat people suffering from PTSD.
Dialectical Behavioral Therapy, first developed in the 1980s by Marsha M. Linehan is a form of psychotherapy derived from Cognitive Behavioral Therapy (CBT). CBT focuses on recognizing the cognitive link – the connection between thoughts, behavior, and feelings, and has been declared to be an efficient therapy in treating health conditions like depression, anxiety disorders, insomnia, and problems with substance abuse.
Trauma-focused DBT is based on CBT but delves deeper into the psychosocial factors involved in the individual’s daily experiences. DBT is used to assist people in coping with distorted or unstable emotional states and harmful behaviors, like self-harm or suicidal tendencies. It is a support-oriented approach to treatment, that allows individuals to dig deeper into their inner self, recognize their strengths, and then build upon them to uplift the person’s impression of themselves and their life, a path towards self-acceptance.
It is a cognitive-based therapeutic model which incorporates identification of thoughts and beliefs that make life difficult, and observe them mindfully until the individual becomes effective in his/her responses. For example, some people believe that if their vulnerability is exposed, it might prove them to be a weak person. Trauma-focused DBT would serve to teach the person, a more appropriate way of building his/her perspective. For example, ‘If I show my vulnerable side to them, they will think I am weak’, would convert to, ‘Vulnerability is human psychology, and everybody experiences it.’
DBT is a collaborative pattern of therapy. In DBT, the therapist-client relationship is always the key to the successful completion of the session. Clients are given worksheets to practice at home, fill diary cards, practice self-soothing techniques, and develop interpersonal effectiveness by role-playing with the therapist.
Skills Training
There are four key skills taught in DBT which individuals can use to cope with distress:
-
Mindfulness
The practice of being present in the current moment, accepting whatever thoughts, feelings, and behaviors that arise without making any efforts to change or control them.
-
Distress Tolerance
Learning how to be mindful in the face of crisis. Here, the person will learn to practice acceptance of how things are, as opposed to how they feel they should be.
-
Interpersonal Effectiveness
Managing self-esteem issues and positive interpersonal relationships while developing the ability to say ‘NO’ and speaking up for yourself.
-
Emotional Regulation
Managing and regulating severe emotions and urges by reducing control over thoughts and actions.
DBT and Trauma
Sufferers of PTSD have difficulty in handling their emotions. They endure problems in maintaining relationships, and sometimes indulge in harmful behaviors, like reckless substance use or self-harm.
Avoidance and PTSD
One of the greatest, most challenging obstacles to recovery from trauma is avoidance. A person dealing with PTSD is often likely to run away from their problems, distressing emotions and uncomfortable situations, they practice avoidance instead of solving the errors of their life. But the truth is, if one continues to suppress his/her emotions, without trying to accept them, healing cannot take place.
With DBT for PTSD, trauma recollections, like distressing feelings, thoughts, memories, people, places, smells, and sights, are not avoided but faced. This is known as exposure and aims to desensitize the individual to objects and situations that once caused them the trauma. This helps them to alleviate their excessive stress and impulsivity and eliminate the elements of mental discomfort. Although this is a very effective DBT technique and has proven to be useful to various PTSD patients, it may not be equally beneficial to some people and can backfire. The good news is, there is nothing to worry about as DBT has tons of other techniques that can be used through the trial and error approach to finally find the right one for yourself.
DBT-Prolonged Exposure(PE) for Trauma
A comprehensive type of treatment using DBT was developed by Dr Melanie Harned to treat PTSD among individuals who are highly affected by trauma and stress.
This is known as DBT Prolonged Exposure (DBT PE) and works by aiming to help individuals stop the avoidance of uncomfortable memories, thoughts, feelings, people, places, and smells that remind them of their trauma. This process includes two forms of exposure; Imaginal, and In Vivo.
Imaginal Exposure involves using one’s imagination to recall the traumatic events and call it aloud in a room, either alone or before the therapist.
In Vivo or ‘real-life’ exposure, involves facing situations and places that have once caused them trauma. This technique is a more direct approach and it’s advised not to attempt unless you have learned a major portion of the DBT for PTSD skills.
Both types of exposure are said to have proved their efficacy in decreasing levels of avoidance, fears, and other trauma-related symptoms.
Research has shown that DBT’s PE is an acceptable, viable, safe, and efficient model for treating PTSD. In fact, according to Harned in her work published in the Journal of Clinical Psychology, ‘74% of clients prefer to receive a combined DBT and PE treatment over either treatment alone.’
DBT-PTSD
In the assessment of DBT’s potential to the treatment of PTSD, researchers from the Central Institute of Mental Health in Mannheim, Germany, conducted a study including 21 female participants who had undergone Childhood Sexual Abuse (CSA). Researchers applied a treatment model known as Dialectical Behavioral Therapy for Post-Traumatic Stress Disorder (DBT-PTSD) – a collaboration of DBT and CBT approaches to PTSD, like exposure therapy.
The reports from the research stated that using DBT-PTSD resulted in vast symptom reductions among the majority of participants with greater pacification of depression and anxiety disorders. Furthermore, the symptoms continued to reduce even after the treatment, up to six weeks. This suggests that the skills taught throughout the DBT-PTSD session had been beneficial outside of a treatment setting.
DBT as a Tool for Approaching Trauma
While more extensive research on the application of DBT for PTSD patients is required, existing research has shown a viable reduction of PTSD symptoms. Dealing with the trauma of any kind can be an extremely painful and challenging experience, so any case-study or research-driven towards improving the quality of life of affected individuals is going to be of great use. DBT takes a comprehensive approach in treating individuals with mental health concerns, and in doing so yields great benefits, which would serve well for anyone, affected by trauma or not.
By improving one’s capacity to develop acceptance through mindfulness, reducing dysfunctional impulsivity through emotional regulation, managing severe urges and underlying emotional triggers through distress tolerance, and learning about how to cope with troublesome encounters with others and use assertiveness and boundaries effectively through interpersonal effectiveness, DBT can teach traumatised individuals invaluable life hacks that will allow them to attain an overall improved quality of life.

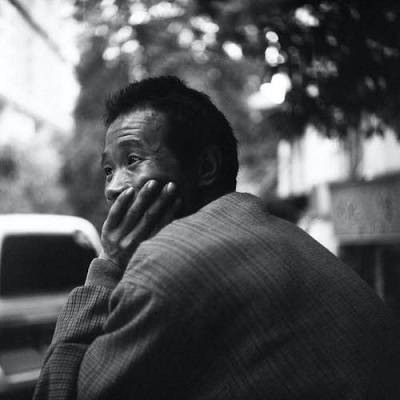
At times, finding help can seem difficult. A lot of us tend to keep it all within ourselves, in the fear of being exposed. Needless to mention, individual therapies can also be very expensive. This is why Swasth has developed a robust platform for people where they can consult trained evidence-based therapy coaches and learn highly effective skills to tackle PTSD or any psychological difficulty via the DBT coach.
-