Background
Depression is a common mental health disorder. It impacts one’s physical, psychological, and social functioning.
There is quite a bit of research involving the benefits of each of the above methods when used independent of each other to treat depression.
Objective
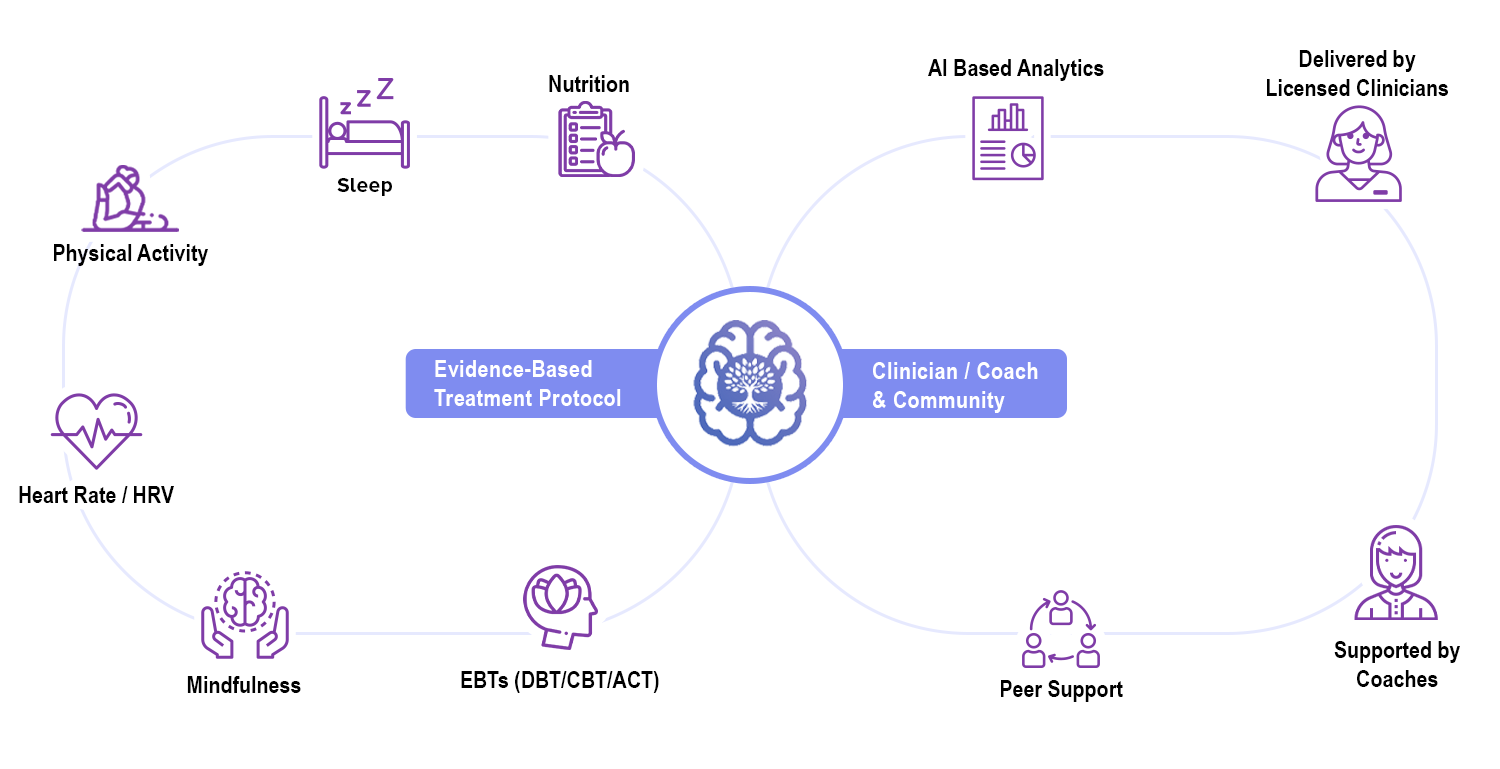
In this article, we explore a holistic approach which combines these methods, delivered via smartphone and supported by a therapist or coach.
Introduction
Depression is a common mental health disorder and one of the leading causes of disease burden and disability worldwide [1-2]. By 2030, depression is predicted to pose the largest burden of disease in high-income countries, surpassing heart disease, dementia, and alcohol-related disorders [1]. Diagnoses of major depression in the U.S. have risen by 33% since 2013, according to US insurer Blue Cross Blue Shield (BCBS) [3].

Although there are several pharmacological treatments for depression, we will focus on psychological interventions in this article.
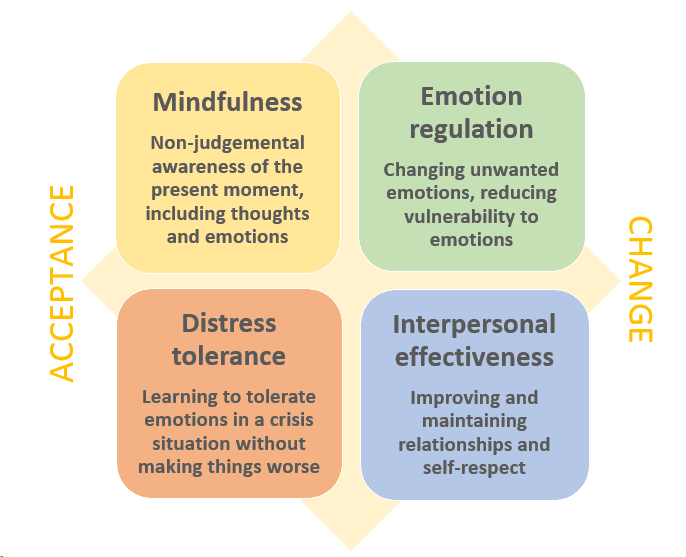
DBT
Across studies, paying attention to and analyzing one's emotions has been found to be both positively and negatively correlated with depression symptoms. Participating in DBT-based skills training may help individuals with treatment-resistant MDD to develop skills that facilitate processing emotions in a way that helps to reduce rather than exacerbate depression symptoms[4]. Skills group participants showed significantly greater improvements in depressive symptoms compared with the control condition[5].
Nutrition
Modifying nutrition factors can be a promising intervention target for mental health. Recent researchs suggests a potential role of nutrition in the development, course, and treatment of depression, whereas present depressive symptoms may also predict the development of an unhealthy lifestyle including poor diet quality. Data supports the hypothesis that high dietary quality is associated with good emotional well-being. This association was particularly evident among females and non-obese middle-aged adults, following adjustments for confounding factors[8].

Heart Rate Variability(HRV)
Reduced HRV has been described in a variety of psychiatric conditions, including bipolar disorder (Lee et al., 2012), schizophrenia (Berger et al., 2010) and attention deficit hyperactivity disorder (Buchhorn et al., 2012). This evidence points to the negative effect of various psychological dysfunctions on the activity of the autonomic nervous system, which appears to be linked to emotion dysregulation (Thayer & Lane, 2009).
Reductions in HRV, specifically in HF variability (parasympathetic modulation), have been reported in major depressive disorder patients in comparison with healthy control subjects. Consistent with this, the LF/HF ratio is higher in these patients than in controls, suggesting a sympathetic prevalence and an overall reduction in HRV (Udupa et al., 2007; van der Kooy et al., 2006).
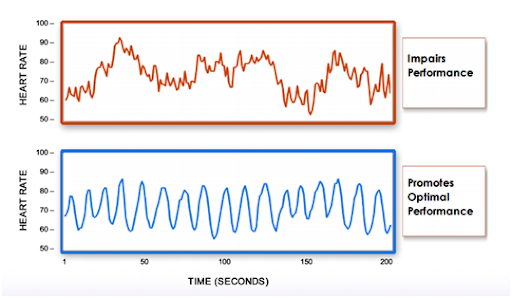
The measurement of HRV allows to assess non-invasively parasympathetic influences and sympathovagal balance at the level of the heart. The available literature indicates that decreased HRV is a valuable marker of cardiovascular morbidity and mortality risk. However, it appears that lowered HRV is tightly linked also with other physical dysfunctions and with a number of psychopathological conditions [9].
Physical Exercise
Throughout history, individuals have noted the mental benefits of exercise and physical activity. Reduction in physical activity over time was also found to be predictive of an increased risk for developing depression. There are numerous challenges that must be overcome before exercise can be used as a treatment in real- world settings. there is substantial evidence supporting exercise use in the treatment of mental disorders, especially depression; however, this research has yet to make an impact on clinical practice[10].
Approach
In this study, we explore an approach combining all the above intervention targets for treating depression. To make it easy for the delivery of care, we propose a smartphone-based, therapist-supported model over a period of 3 months.
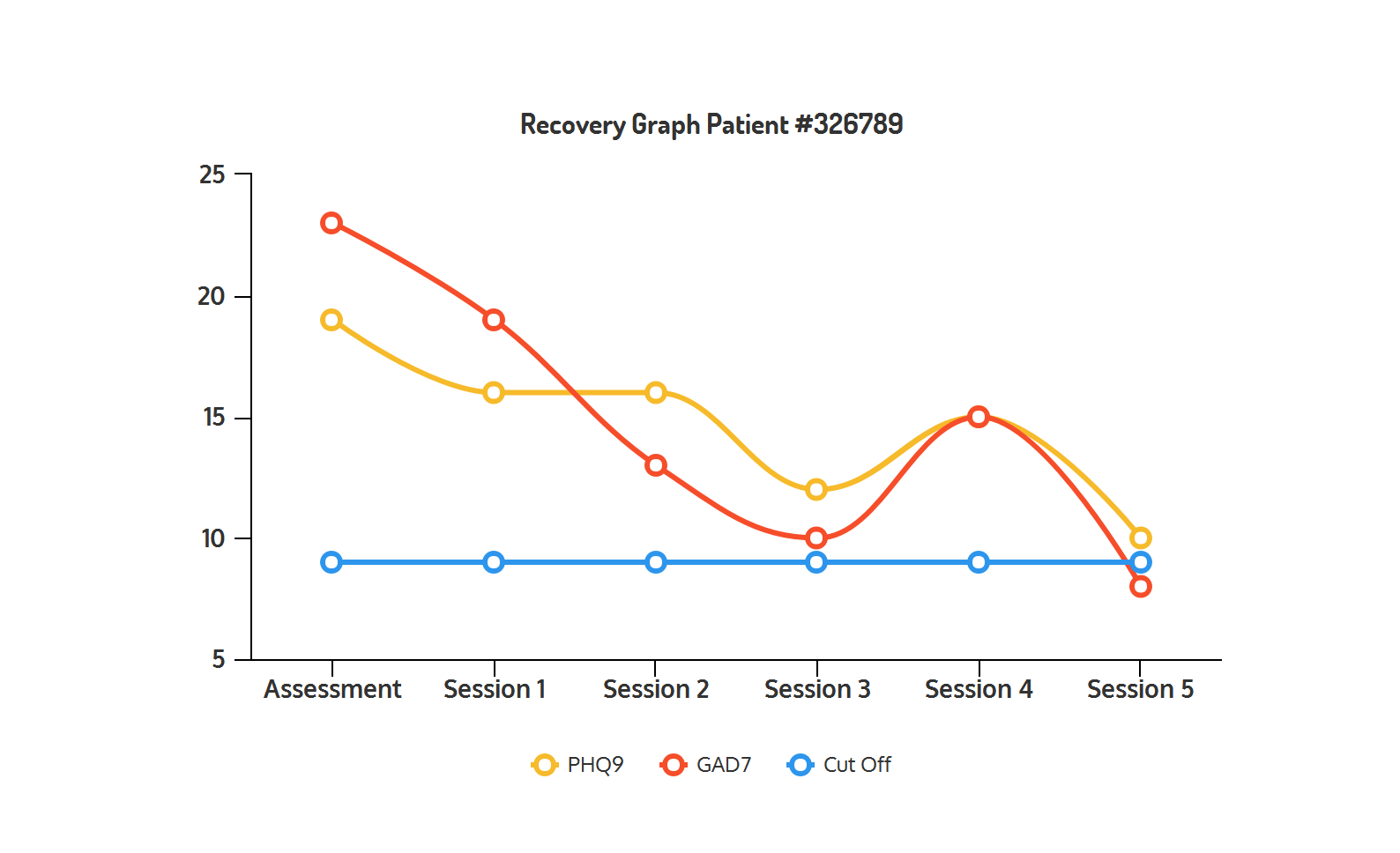
We could then assess improvements in depression during the course as well as end of treatment. This could be measured by standardized assessments such as Patient Health Questionnaire-9 [PHQ-9] and the Generalized Anxiety Disorder [GAD-7} scales.
DBT Coach App
We have developed a smart phone app (available both on iOS and Android platforms) called DBT Coach.

The app enables:
- Clinicians to deliver DBT electronically
- Clients to track moods and do DBT diary card entries daily
- Clients to log Nutrition entries daily (including macro and micro nutrients by integrating with a comprehensive third-party nutrient database)
- Clients to log sleep
- Clients to perform breathing exercises (and import HRV entries)
- Integrates with Apple Health, Fitbit and GoogleFit
Using advanced AI techniques, DBT Coach extracts important pieces of context from exercise and journal entries and suggests skills that best work in a particular situation given the context.
If you are a clinician interested in a Behavioral Health Platform built for Evidence-Based treatment approaches please contact us at info@resiliens.com.
References
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006 Nov;3(11):e442 [FREE Full text] [CrossRef] [Medline]
- Richards D. Prevalence and clinical course of depression: a review. Clin Psychol Rev 2011 Nov;31(7):1117-1125. [CrossRef] [Medline]
- World Economic Forum. (2011). Depression is the no. 1 cause of ill health and disability worldwide. Retrieved from link.
- Feldman G., Haley R. Change in emotional processing during a dialectical behavior therapy-based skills group for major depressive disorder. Volume 47, Issue 4, April 2009 [CrossRef]
- Harley, R. Sprich, S. Adaptation of Dialectical Behavior Therapy Skills Training Group for Treatment-Resistant Depression : February 2008 - Volume 196 - Issue 2 [CrossRef]
- Therese Waterhous, PhD, RD, LD Nutrition Intervention in the Treatment of Eating Disorders. Retrieved from link
- Rahe C., Berger K. (2016) Nutrition and Depression: Current Evidence on the Association of Dietary Patterns with Depression and Its Subtypes. In: Baune B., Tully P. (eds) Cardiovascular Diseases and Depression. Springer, Cham [CrossRef]
- Meegan AP, Perry IJ, Phillips CM. The Association between Dietary Quality and Dietary Guideline Adherence with Mental Health Outcomes in Adults: A Cross-Sectional Analysis. Nutrients. 2017;9(3):238. Published 2017 Mar 5. [CrossRef]
- Andrea Sgoifo, Luca Carnevali, Maria de los Angeles Pico Alfonso & Mario Amore (2015) Autonomic dysfunction and heart rate variability in depression, Stress, 18:3, 343-352, DOI: 10.3109/10253890.2015.1045868
- Rethorst, C. D. (2019). Effects of exercise on depression and other mental disorders. In M. H. Anshel, S. J. Petruzzello, & E. E. Labbé (Eds.), APA handbooks in psychology series. APA handbook of sport and exercise psychology, Vol. 2. Exercise psychology (p. 109–121). American Psychological Association. https://doi.org/10.1037/0000124-006